Gastroenterological Procedures
Diagnostic Procedures
Oesophago-Gastro-Duodenoscopy

Colonoscopy

Enteroscopy of the small bowel

Capsule Endoscopy of the small bowel

Endoscopic Retrograde Cholangio-Pancreatography (ERCP)

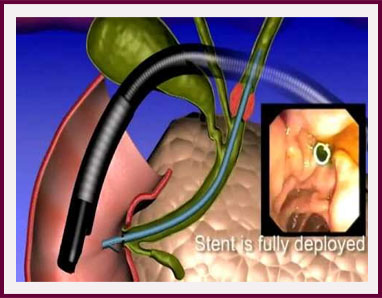
This endoscopic examination method is used to examine the bile ducts, which connect the liver to the small intestine and the pancreas. The endoscope is a side viewer called a Duodenoscope and is passed through the mouth, past the stomach and into the second part of the upper small intestine or duodenum. The Ampulla of Vater, which is the entrance to the bile and pancreatic ducts, is located and a catheter is used to enter the common bile duct or pancreatic duct. Contrast (a dye that is visible on x-ray) is injected and by Fluoroscopy (live, real-time x-ray scanning) these ducts can be examined. This examination is done if the bile ducts are thought to be blocked by gallstones or a tumour.
Liver Biopsy

Liver biopsy may be performed to diagnose inflammation, liver scarring (cirrhosis), cancerous or non-cancerous growths or some infections in the liver. Liver biopsy involves removing a tiny piece of liver tissue under a local anaesthetic, using a special liver biopsy needle. The specimen is then sent for pathological examination. Ultrasound scanning is commonly used to locate the best and safest place to insert the biopsy needle.
Therapeutic Procedures
By gastroscopy
Dilatation of oesophageal strictures

Insertion of oesophageal stents

Injection sclerotherapy and band-ligation of oesophageal varices

Insertion of percutaneous endoscopic gastrostomy (PEG) feeding tube

Haemostasis (excluding oesophageal varices which is discussed elsewhere)

Laser or Argon-Plasma Beam re-canalisation

By Colonoscopy
Removal of polyps

Haemostasis (stopping bleeding) of bleeding lesions

Insertion of stents

Laser re-canalisation of inoperable colon cancer

Treatment of haemorrhoids

Haemorrhoids or piles are dilated blood vessels under the lining of the lower rectum. They may become inflamed and painful or they may bleed. They can be of different severity levels, defined by whether they remain internal (Grade 1), prolapse outside of the anus but are reducible (can spontaneously go back inside or be pushed back by a finger) (Grade 2) or prolapse outside and become stuck in that position, with persistent painful inflammation and bleeding (Grade 3). Grade 1 and 2 haemorrhoids are generally treatable without major surgery. They can be treated by either ligation or injection sclerotherapy. Ligation is done by placing rubber bands around the base of the piles causing them to die, shrink and fall off. Injection sclerotherapy involves using a flexible Colonoscope through which an injection catheter is advanced and special medicines are accurately injected into each pile. This medicine causes the blood vessels to inflame, shrink and scar up.
By ERCP
Sphincterotomy and extraction of gallstones from the bile ducts

Stenting of the bile ducts or pancreatic duct

Conversion of external-internal biliary stent to endoscopic stent ('rendezvous procedure')